Knowledge Center
Debunking Myths About TMS Therapy: Separating Fact from Fiction
Transcranial magnetic stimulation (TMS) therapy is a non-invasive treatment that uses magnetic fields to stimulate specific areas of the brain. It has been shown to be an effective treatment for a variety of mental health conditions, including depression, anxiety, and OCD. However, despite its proven effectiveness, there are many myths and misconceptions surrounding TMS therapy. In this post, we will separate fact from fiction and debunk some of the most common myths about TMS therapy. Click the picture to read the full post.
March 3rd, 2023
What is the Dip?
Transcranial magnetic stimulation (TMS) therapy has emerged as a promising treatment for a variety of mental health conditions, including depression, anxiety, and OCD. However, not all patients who undergo TMS therapy experience the same level of improvement. In fact, some patients may experience a temporary worsening of their symptoms before they begin to improve, a phenomenon known as "the dip." Click the picture to read the full post.
February 24th, 2023
What is TMS?
Transcranial Magnetic Stimulation (TMS) is a non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain. It has gained popularity in recent years as an effective treatment for several neurological and psychiatric disorders. In this blog post, we will explore TMS in-depth, its benefits, what it typically treats, and other essential information. Click the picture to read the full post.
February 17th, 2023
Debunking Myths About TMS Therapy: Separating Fact from Fiction
Transcranial magnetic stimulation (TMS) therapy is a non-invasive treatment that uses magnetic fields to stimulate specific areas of the brain. It has been shown to be an effective treatment for a variety of mental health conditions, including depression, anxiety, and OCD. However, despite its proven effectiveness, there are many myths and misconceptions surrounding TMS therapy. In this post, we will separate fact from fiction and debunk some of the most common myths about TMS therapy.
Click the picture to read the full post.
March 3rd, 2023
What is the Dip?
Transcranial magnetic stimulation (TMS) therapy has emerged as a promising treatment for a variety of mental health conditions, including depression, anxiety, and OCD. However, not all patients who undergo TMS therapy experience the same level of improvement. In fact, some patients may experience a temporary worsening of their symptoms before they begin to improve, a phenomenon known as "the dip."
Click the picture to read the full post.
February 24th, 2023
What is TMS?
Transcranial Magnetic Stimulation (TMS) is a non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain. It has gained popularity in recent years as an effective treatment for several neurological and psychiatric disorders. In this blog post, we will explore TMS in-depth, its benefits, what it typically treats, and other essential information. Click the picture to read the full post.
February 17th, 2023
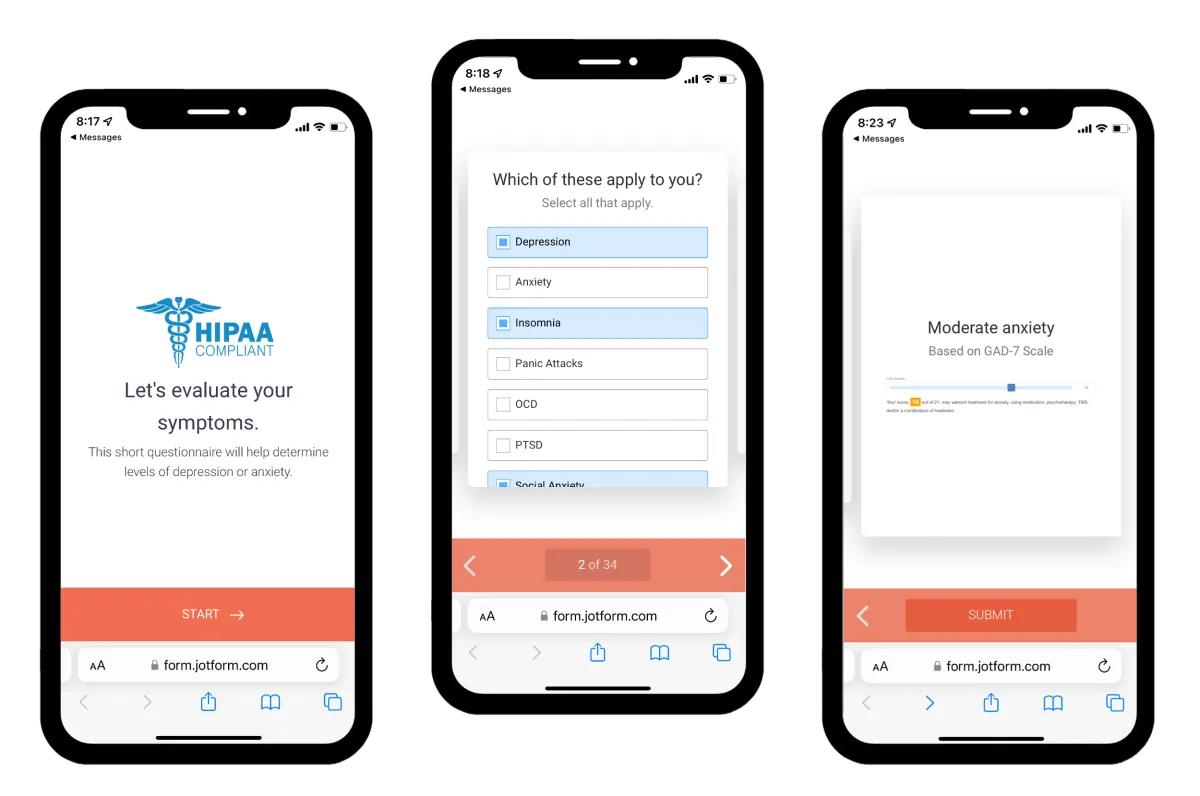
Not sure if you need any of this?
Not sure if you need any of this?
Find out by taking this short assessment
Secure and confidential.
Or
Contact Info
Business Hours
Mon-Fri: 8am - 4pm
Sat/Sun: Closed
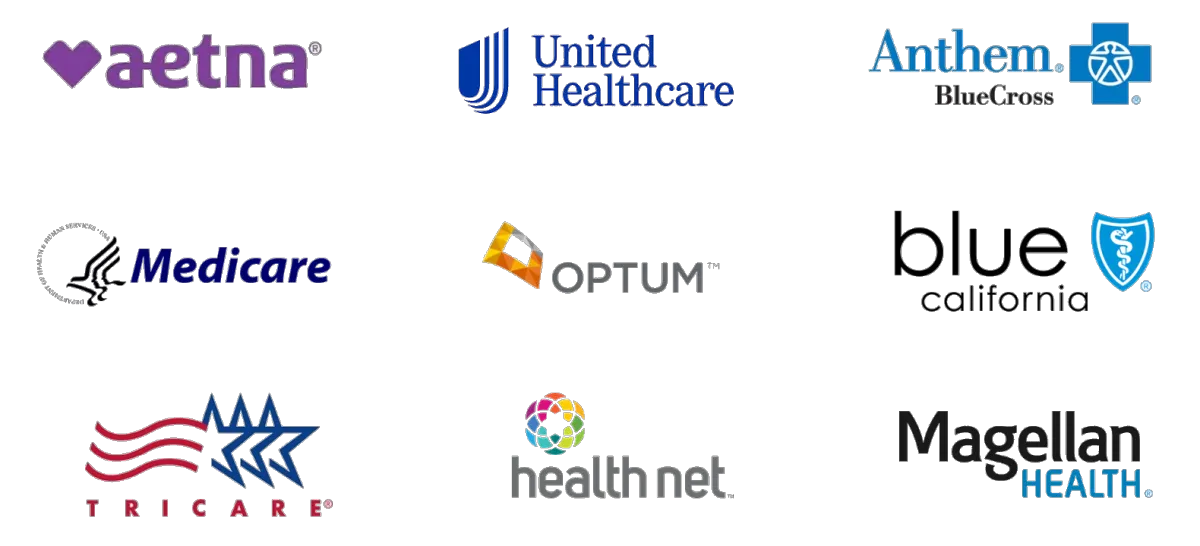
Insurances we accept
Ⓒ 2023 —caltms.com — All rights reserved